New targets for CAR-T cell therapy against acute myeloid leukemia through AI-assisted analysis
Interdisciplinary cooperation between LMU and Helmholtz Munich supported by Bavarian Research Foundation
Unlike other forms of blood cancer, acute myeloid leukemia (AML) cannot currently be treated with CAR-T cell immunotherapy. The reason is that specific molecular targets with which certain immune cells could specifically target AML cells are lacking, which would permit the immune system to attack cancer. Two research teams of Professor Dr. Sebastian Kobold with Dr. Adrian Gottschlich from the Division of Clinical Pharmacology at LMU University Hospital Munich and Dr. Carsten Marr with Moritz Thomas from the Institute of AI for Health at Helmholtz Munich have now succeeded in discovering such targets. The results have now been published in the journal Nature Biotechnology.
AML – one of several forms of leukemia (“blood cancer”) – is a treacherous disease. Five years after the initial diagnosis, only one-third of patients are still alive. Up to 85 percent of patients appear to be cured after intensive chemotherapy. However, in more than half of them, the disease returns within one to two years because the chemotherapy has not destroyed all leukemia cells. In the event of a relapse, a stem cell transplant is the only hope for cure for a patient. But even then, the long-term probability of survival is less than 20 percent. New treatment options are therefore urgently needed.
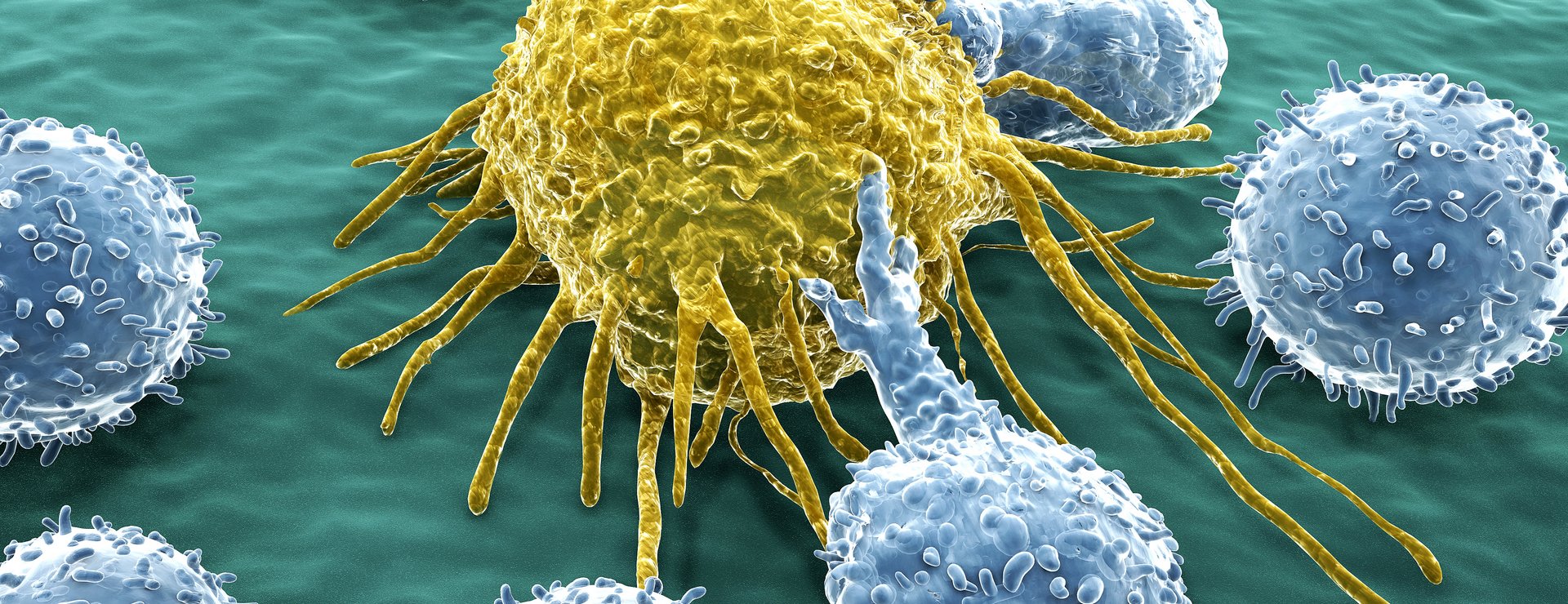
CAR-T cell therapy is an innovative therapy. CAR-T stands for “chimeric antigen receptor in T cells”. T cells are cells of the immune system. Cancer cells evade their “normal” attempts to attack them by using various molecular tricks. Thus, T cells no longer recognize their opponents, the cancer cells. During CAR-T cell therapy, T cells are first removed from the patients and then genetically engineered to produce a specific protein (CAR) on their surface. When these CAR-T cells are injected back into the patient’s body, these will only engage their target: CD19, which ensures that they recognize the patient’s cancer cells and bind to them in a targeted manner. The cancer cells consequently die.
New Targets
However, the approved CAR-T cells against CD19 are not suitable for AML, because CD19 is (usually) not present on the surface of AML cells. Clinical results with CAR-T cells directed against other surface molecules of AML cells have been sobering so far, according to scientists. This is because CAR-T cells were unable to distinguish between healthy and degenerated cells – with correspondingly induced significant side effects.
The physician Sebastian Kobold and the physicist Carsten Marr, together with colleagues from the LMU University Hospital Munich and the Institute of AI for Health at Helmholtz Munich, set out to find alternative molecules that would ideally be found exclusively on the surface of AML cells. With the help of extensive bioinformatic analyses and the integration of expression data from more than half a million individual cells, two candidates finally crystallized out of 25,000 potential cell surface molecules. These are known as CSF1R and CD86. “Such an analysis would not have been possible a few years ago, since the required single-cell data has been generated only very recently,” says Marr, who led the AI-assisted analysis in the study at Helmholtz Munich.
The researchers produced CAR-T cells in the laboratory of the LMU University Hospital Munich that precisely target these molecules. The cells were then tested on different AML models, including AML cells from patients. The results, according to Kobold are promising: “On the one hand, these CAR-T cells are effective against AML, but on the other hand, they hardly destroy healthy cells.”
The study impressively demonstrates how the synergy of interdisciplinary research groups can lead to breakthroughs in health research to treat patients in the best possible way. The researchers’ next goal: They want to develop GMP (good manufacturing practice)-capable processes to produce CAR-T cells that can then also be used in clinical trials with AML patients. This is to take place within the framework of the “Bavarian Cell Therapy Catalyst”, which is supported by the Bavarian Research Foundation. Kobold expects the first tests with patients in two to three years.
Original publication
Gottschlich et al. (2023): Single-cell transcriptomic atlas-guided development of chimeric antigen receptor (CAR) T cells for the treatment of acute myeloid leukemia. Nature Biotechnology, DOI: 10.1038/s41587-023-01684-0







