Machine Learning How AI is Revolutionizing Medicine
Computer systems can already independently analyze health data, learn from it and even derive therapy recommendations. Which opportunities this means for patients and what research needs to apply artificial intelligence in practice.
Some data is generated all the time in the healthcare system: Blood pressure measurements, blood values, oxygen saturation, ultrasound and MRI scans. They are evaluated, used for diagnosis, and archived. But what if computer systems could learn independently from the collected data of a patient, even develop new insights from it? The use of artificial intelligence in medicine will be one of the dominant topics in health research over the next few years. Where do we stand - and what are the prospects?
The computer can learn “supervised”
Artificial intelligence describes the ability of computer programs to learn. There are two paths for this learning.The first involves “supervised learning”. Researchers show the computer a large number of similar things, teaching it what is right or wrong, healthy or sick, depending on the question. The idea behind this: If the computer gets enough input, it can eventually make the distinction itself. In this way, it can not only take a lot of work off the hands of physicians, it can also improve the quality of diagnosis and treatment.
What is machine learning? (in German)
Audio File
In this podcast, Julia Schnabel explains how machine learning works and why the term is not ideal.
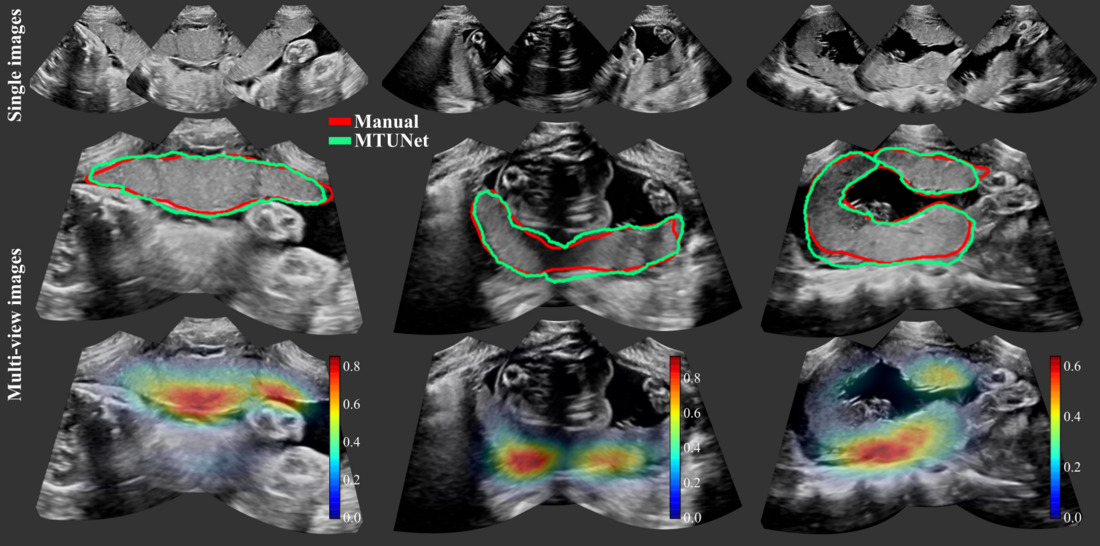
Making early diagnoses from ultrasound images
A practical example: Julia Schnabel and her research group are training an algorithm to measure the placenta in pregnant women. The placenta provides nourishment for the unborn child in the womb. If the placenta is too small, the unborn child will not receive enough supply. The child may have to be delivered earlier to prevent permanent damage. However, because it has been difficult to determine the size of the placenta and its ability to provide nourishment, doctors pay particular attention to the growth of the child during check-ups - a potential undersupply therefore only becomes visible through its subsequent effects.
The computer as a sparring partner for the doctor
The approach worked: The computer program not only measures the size of the placenta quite well. "We fed our algorithm with additional data so that it also recognizes organs and body parts of the unborn child," Schnabel explains. The goal is not to replace the experts, but to support them: "When it comes to assessing whether a child should be delivered earlier or not, a doctor will always decide the future. However, thanks to computer algorithms, experts will have a better basis for their decision in the future. In this way, a clever artificial intelligence could become a kind of sparring partner for the experts in some areas in the future. The placenta measurement by Schnabel's team is a typical example of how artificial intelligence could advance medicine, and in some areas downright revolutionize it: The computer is fed data, learns, and delivers insights that bring new knowledge to people.
Data for Prevention (in German)
Audio File
In this podcast, Julia Schnabel explains how data could help detect diseases earlier.
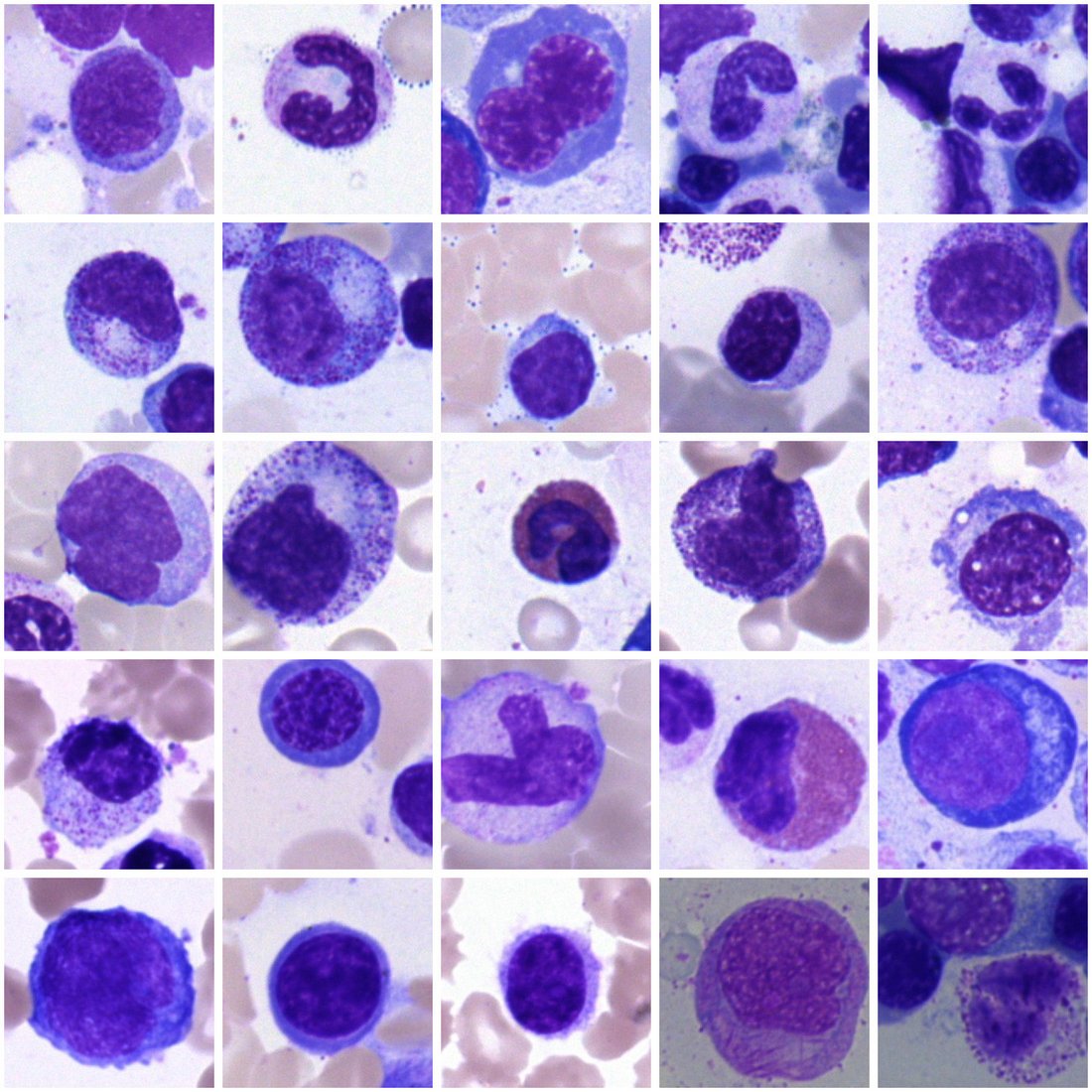
Digitalized blood analysis
Carsten Marr and his colleagues are taking a similar approach. The researchers focus on tasks for which specialists normally spend hours and days at the microscope: When blood cancer is suspected, several hundred cells in a so-called blood smear are examined and classified by histologists. The results show whether and to what extent the patient is actually suffering from a similar disease, for example, blood cancer, and how a possible treatment can proceed.
Marr and his team fed a so-called neural network with hundreds of thousands of images of individual white blood cells and the information of the cell type. And with success; the cell type predictions Marr's program makes on new images are as good as the histologists' results. "A neural network is a kind of black box. It learns and can then classify new cells itself, but we don't know in detail what criteria it uses to decide," Marr says. That is why he is currently working to better understand these criteria: "The criteria can not only be helpful for histologists. It is also important for us to understand the decision-making process in order to avoid possible mistakes and learning in the wrong direction. In medicine, in particular, it's about using this black box of machine learning, but also understanding what makes it tick," Marr adds. Only then could computers become trustworthy assistants for physicians.
Image Gallery
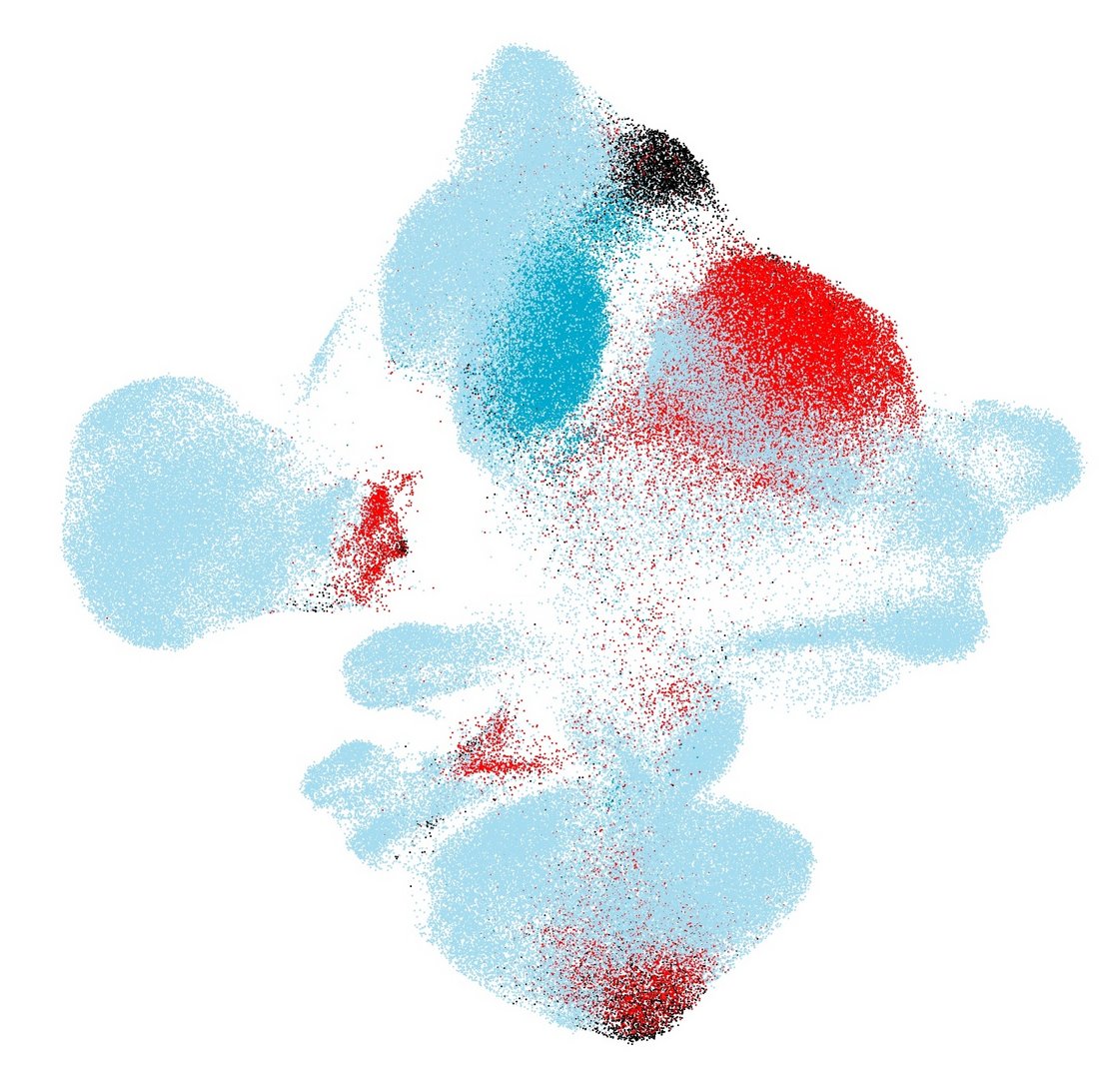
“Unsupervised” learning
There is a second way to apply artificial intelligence: Here, the computer receives as little assistance as possible; it should be able to learn without supervision. Mathematician Fabian Theis uses this method, for example, in what is known as single-cell analysis: The computer receives data on individual cells and their metabolism - and has to find patterns in them. “We don't tell it what is right or wrong, we just give it some additional information. Ideally, it finds out what similarities there are in certain properties,” explains Theis.
In practice, this could soon mean: The computer compares the metabolism of cells in the pancreas of people with diabetes with the metabolism of cells in the pancreas of healthy people, and finds out what is different about the defective cells of the diabetes patients. In the next step, specific drugs can then be sought in the future to repair the corresponding cell metabolism changes.
Data difficult to access
In order to achieve breakthroughs, research requires enormous amounts of data. And this data is not always available in Germany, as Julia Schnabel also reports: “Ultrasound images of the placenta can still be obtained reasonably well; doctors ask patients for their consent and record the ultrasound examination. For many other data, however, it's difficult to get the information in a consistent, comparable format in Germany.” That's mainly because the health care system in this country is enormously fragmented. Each state has its own health ministry, and each hospital collects data in its own way.
“In Germany, on the other hand, there is a real obsession with data protection,” says Carsten Marr. “What amazes me is the discrepancy: Everyone throws personal information around on social networks, but when it comes to medical data that is supposed to be used for research, you have to overcome countless hurdles,” says Marr. He himself considers data protection enormously important, but this alone rarely stands in the way of research, he says: “Researchers aren't interested in the names, but in the information behind them.” Nevertheless, he and his colleagues experience time and again that it is very difficult to obtain medical data for research if it is available at all.
And if there isn't enough data available in this country for the scientists to conduct research with? For Fabian Theis, that's not an obstacle: “At the moment, you have to be pragmatic; especially in collaborations with foreign research institutions, the data often comes from there, too,” says Theis. However, he is optimistic that there will also be a jolt forward in Germany in terms of data provision soon. “I consult on the topic in numerous political committees and I see a real will for progress there,” says Theis. That would be a win-win-win situation: For research, for patients, and for Germany as a research location.
Latest update: June 2022.